A 58y/o female
A 58y/o female came to the casuality with the chief complaints of:
1. Sudden onset chest pain
2.Giddiness
3. Profuse sweating
1 episode at 6:00 PM on 08/09/21
The chest pain is throbbing type in the epigastric region with giddiness, sweating. A/w 1 episode of vomiting - non bilious, non projectile, with food as the content, not a/w palpitations, blackouts, blurring of vision, diplopia, headache, neck pain.
The patient went to local RMP with the same complaints. There her GRBS was 446mg/dl for which Tab Metformin 500mg was given and the patient was referred to our hospital for further management. On
presentation, her vitals were Afebrile BP 120/70mmHg PR 78bpm RR 12cpm SpO2 96%GRBS 336
Past History: The patient was apparently symptomatic 4 years ago. Then she had altered sensorium, she had no orientation of time, place and person for 1 day and was diagnosed with HTN and Type 2 DM in our hospital. MRI Brain - Acute infarct in R lentiform nucleus and internal capsule
USG Abdomen - Grade 1 fatty liver Carotid Doppler - Atherosclerotic changes in B/L carotid arteries K/C/O DM since 4 years Tab Glimi 0.5mg and Tab Metformin 500mg OD HTN since 4 years Tab Telma 40mg. The patient is an agricultural labourer by occupation.
Personal History: Reduced appatite Takes mixed diet Regular bowel and bladder movements No addictions
General Examination: Patient is Moderately built and nourished. No pallor, icterus, cyanosis, clubbing, lymphadenopathy, pedal oedema Afebrile BP 90/70 mmHg PR 78 bpm RR 12 cpm SpO2 96% GRBS 336.
Systemic examination:
CVS: S1 S2 +RS BAE +P/A shape obese,
tenderness in the epigastric region, no palpable mass.
CNS: Patient is conscious speech normal GCS 15/15 Cranial nerves normal
Motor system: normal
Sensory system: normal
Reflexes: R L Biceps + +Triceps --Supinator --Knee 3+ 3+Ankle + +Plantar Flexor flexor
Investigations:
1. RBS 440MG/DL
2. HEMOGRAM - HB 9.2, TLC 13300, PCV 27, PLT 2.07 LAKH
3. CUE ALB TRACE, SUGARS ++++, PUS CELLS 3-4, EPI CELLS 2-3
4. URINE ELECTROLYTES NA 382, K 33.3, CL 488
5. BGT A+
6. CHEST X RAY BEDSIDE
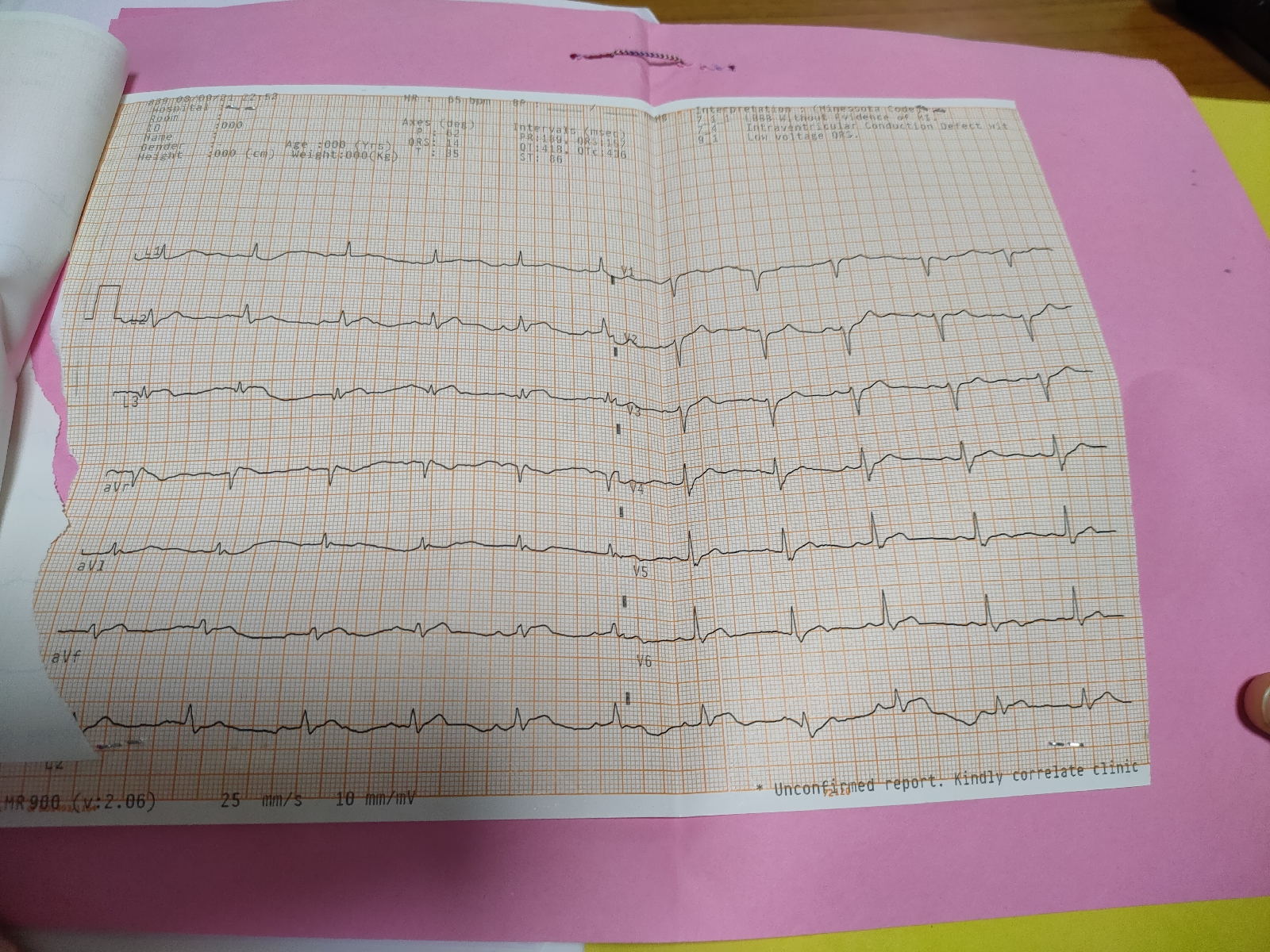
7. ECG BEDSIDE
8. LFT TB 1.04, BD 0.35, AST 37, ALT 19, ALB 3.7, ALP 279, PROT 6.4
9. RFT CR 1.0, UREA 33, NA 137, K 3.9, CL 102
Treatment Given:
1. IVF NS AT 20ML/KG/HR
2. INJ OPTINEURON 1 AMP IN 100ML NS
3. INJ HAI 6 U ACTRAPID IV STAT
4. INJ PANTOP 40 MG IV STAT
5. TAB PCM 500MG PO TID
6. TAB ULTRACET 1/2 1/2 1/2 1/2
7. TAB ASPIRIN 325 MG
8. TAB CLOPITAB 300 MG
9. TAB ATORVAS 80 MG
10 GRBS MONITORING WITH INJ HAI INFUSION AT 8ML/HR
3 AM 559 MG/DL
4 AM 491 MG/DL
5 AM 409 MG/DL
6 AM 393 MG/DL
At the time of admission
6 am
F/U:
Patient was discharged from the hospital on 09/09/21 at 6:30am and was referred to a higher centre.
The patient got admitted into another hospital. She presented with acute pulmonary edema, grade 4 dyspnoea, she got intubated in casuality. Then was shifted to the ICU after stabilisation Angio was done PTCA was placed. Then she got discharged.